CORNEA TRANSPLANTS
CORNEA TRANSPLANTATION

Cornea transplantation is the most frequently performed transplant worldwide. Approximately 40,000 cornea transplants are performed in the United States annually. The cornea is the front surface of the eye and is responsible for two thirds of the focusing power of the eye. It is primarily made of layers of collagen in ordered rows that allow light to pass through. Injury, infections, and disease can cause the cornea to lose its transparency and result in a loss of vision.
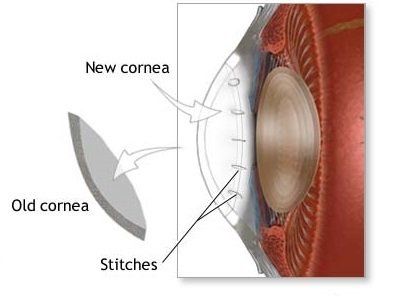
Cornea transplants have traditionally involved surgically removing the central diseased portion of a patient’s cornea and replacing it with a full-thickness donor cornea obtained from a recently deceased individual whose corneas have been stored in an eye bank. This is performed as outpatient surgery and takes anywhere from 40 minutes to an hour or more depending upon what else needs to be done such as cataract removal, intraocular lens implantation, or repair of the iris. Recovery of best vision usually takes 4 to 6 months. The patient has a life-long risk of graft rejection.
The main disadvantages to this surgery are the introduction of astigmatism and the unpredictability of the eye’s refractive error afterwards. This is because the curvature of the donor cornea is unknown prior to surgery and the corneal curvature greatly affects the eye’s refractive error.
DSEK
(DESCEMET’S STRIPPING ENDOTHELIAL KERATOPLASTY)

This procedure is designed to replace the damaged or abnormal corneal endothelium (inner cell lining on the cornea) when a patient has decreased visual acuity from corneal swelling. Previously these patients would require a full penetrating corneal transplant, but new technology allows for replacement of only the abnormal endothelium. This results in much faster visual recovery, leaving the patient with a stronger cornea and less astigmatism than what commonly occurs with a traditional transplant.
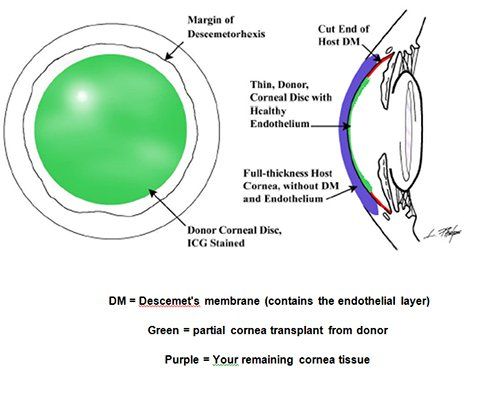
During the procedure a small incision is made and the diseased endothelium and Descemet’s membrane are removed from the inner surface of the patient’s cornea. A disc of tissue is then taken from the inner layer of a healthy donor cornea, folded gently and inserted into the anterior chamber. An air bubble is introduced to push the tissue into place where it eventually heals into a stable position. Typical post-operative results are in the 20/20-20/40 range and patients notice less glare and improved contrast sensitivity.
INDICATIONS:
- Fuch’s endothelial dystrophy
- Pseudophakic bullous keratopathy
- Other cause of endothelial failure
- Minimal corneal scarring
- Best acuity 20/40 or worse
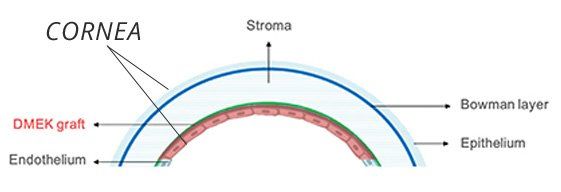
DMEK
(DESCEMET'S MEMBRANE ENDOTHELIAL KERATOPLASTY)

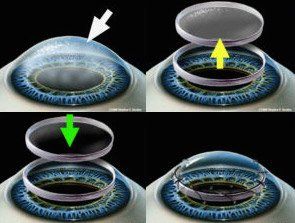
Descemet's Membrane Endothelial Keratoplasty, or DMEK, is an exciting new method of corneal transplantation that we are pleased to offer at Helm Vision Group. What makes this procedure unique is that it utilizes thinner donor tissue (it does not include any stromal tissue) which decreases potential for graft rejection and expedites the recovery process. This procedure has proven to result in faster recovery than DSEK and results are clear in as little as a few weeks.
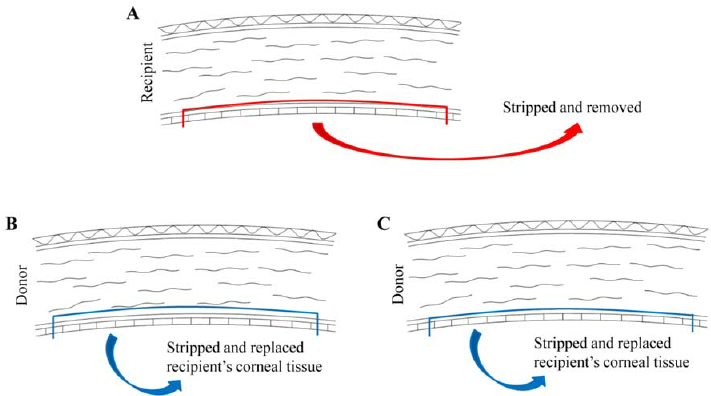
The above image (left) compares DSEK (A and B) and DMEK (A and C). DMEK utilizes thinner donor tissue than DSEK.
In comparison to DSEK, DMEK is a much newer procedure that provides a faster rate of visual recovery and a higher potential for 20/20 or better vision. As with any surgery, there are pros and cons and potential risks. Talk with Helm Vision Group to determine whether DMEK or DSEK is right for you.
PROS AND CONS:
Pros:
Faster recovery time
Lower risk of rejection
Proven to have better success than DSEK
Cons:
Longer back-positioning after surgery
May not be possible to do successfully in someone who has neck problems and cannot position their face flat
May not be possible to do in eyes with previous glaucoma or retinal surgery
INTACS®

Intacs prescription inserts are indicated for use in the correction of near-sightedness and astigmatism for patients with keratoconus, where contact lenses and glasses no longer provide adequate vision.
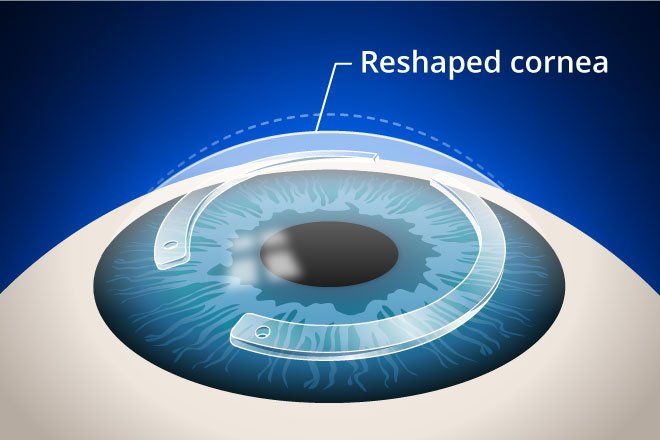

Keratoconus is a progressive eye disease, which causes a thinning of the cornea, the clear front surface of the eye. As the disease progresses, the quality of vision deteriorates. For some, contact lenses or glasses are a satisfactory solution, but for others, Intacs may be the best possible option for improving vision.
Intacs prescription inserts are approved by the FDA for keratoconus under a Humanitarian Device Exemption (HDE).
Corneal collagen crosslinking is an exciting new option to treat keratoconus with UV light in order to prevent progression. It frequently results in improved vision but in most cases keeps it from getting worse.

